For appointment and information, you can rich us on +90532 433 6003(whatsapp)
 Obstetrician, Gynecologist, Genital Esthetic Surgeon in Turkey
Obstetrician, Gynecologist, Genital Esthetic Surgeon in TurkeyFor appointment and information, you can rich us on +90532 433 6003(whatsapp)
 Obstetrician, Gynecologist, Genital Esthetic Surgeon in Turkey
Obstetrician, Gynecologist, Genital Esthetic Surgeon in Turkey
Barrier methods of birth control are physical or chemical barriers that prevent sperm from passing through the woman’s cervix into the uterus and fallopian tubes to fertilize an egg. Some methods also protect against sexually transmitted disease (STDs).
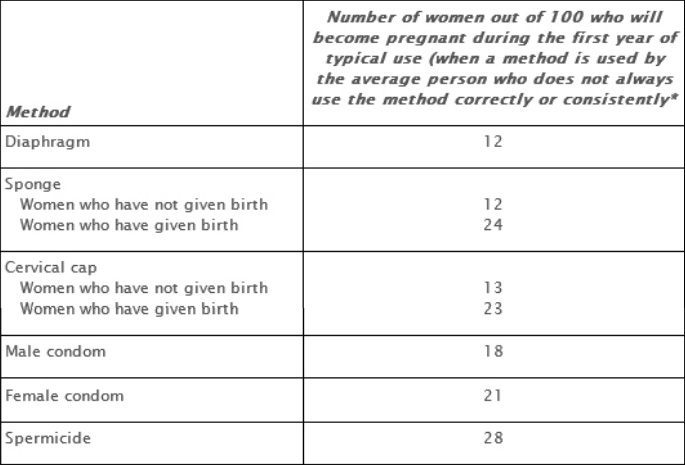
The following table lists the barrier methods and their effectiveness in preventing pregnancy;
A spermicide is a foam, cream, jelly, suppository (an insert that melts after it is inserted in the vagina),or film (thin sheets). Spermicide can be used with all other barrier methods except the sponge, which already contains a spermicide.
A spermicide should be inserted into the vagina close to the cervix no more than 30 minutes before intercourse. It should remain in place for 6–8 hours after sex. A spermicide should be reapplied with each act of sex.
1. Benefits;
2. Risks;
3. Possible side effects; allergic reaction to the spermicide and vaginitis.
Two types of condoms are available: male and female. The male condom is a thin sheath made of latex (rubber),polyurethane (plastic),or natural (animal) membrane that is worn by the man over his erect penis. Latex and polyurethane condoms provide the best available protection against many STDs, including HIV.
The female condom is a thin plastic pouch that lines the vagina. It is held in place by a closed inner ring at the cervix and an outer ring at the opening of the vagina. It can be inserted up to 8 hours before sex and provides some protection against STDs.
Both types of condoms should be used with a lubricant to prevent the condom from tearing or breaking and to reduce irritation. Latex condoms should only be used with water-based or silicone lubricants. Oil-based lubricants can weaken the latex and increase the risk that the condom will break.
1. Benefits;
2. Risks; none
3. Possible side effects; allergic reaction to latex or polyurethane.
The sponge is a doughnut-shaped device made of soft foam coated with spermicide. It is inserted into the vagina to cover the cervix. It is available without a prescription. The sponge does not protect against STDs, including HIV. A male or female condom should be used with the sponge to provide STD protection if you are at risk of getting an STD.
1. Benefits; - It can be bought over-the-counter.
2. Risks; - Cases of toxic shock syndrome have occurred in a few women using the sponge.
The sponge should only be used if you are at low risk of HIV infection. Frequent use of spermicides can increase the risk of getting HIV from an infected partner.
3. Possible side effects; vaginal irritation and allergic reactions to polyurethane, spermicides, or sulfites (all of which are found in the sponge).
What is the diaphragm and how is it used?
The diaphragm is a small dome-shaped device that fits inside the vagina and covers the cervix. It is used with spermicide. Diaphragms are made of latex or silicone. They require a prescription and need to be fitted by a health care provider. Use water-based lubricants only if you use a latex diaphragm.
The diaphragm does not protect against STDs, including HIV. A male or female condom should be used with the diaphragm to provide STD protection if you are at risk of getting an STD.
1. Benefits;
2. Risks;
3. Possible side effects; allergic reaction to latex or to the spermicide.
The cervical cap is a small plastic dome that fits tightly over the cervix and stays in place by suction. The cervical cap is used with a spermicide.
It has a strap over the dome that is used for removal. A cervical cap must be fitted and prescribed by a health care provider.
The cervical cap does not protect against STDs, including HIV. A male or female condom should be used with the cervical cap to provide STD protection if you are at risk of getting an STD.
1. Benefits;
2. Risks;
3. Possible side effects; allergic reaction to the spermicide and vaginal irritation or odor.
Long-acting reversible contraception (LARC) methods include the intrauterine device (IUD) and the birth control implant. Both methods are highly effective in preventing pregnancy, last for several years, and are easy to use. Both are reversible—if you want to become pregnant or if you want to stop using them, you can have them removed at any time.
The IUD and the implant are the most effective forms of reversible birth control available. During the first year of typical use, fewer than 1 in 100 women using an IUD or an implant will become pregnant. This rate is in the same range as that for sterilization.
Over the long term, LARC methods are 20 times more effective than birth control pills, the patch, or the ring.
The IUD is a small, T-shaped, plastic device that is inserted into and left inside the uterus. There are two types of IUDs:
Both types of IUDs work mainly by preventing fertilization of the egg by the sperm. The hormonal IUD also thickens cervical mucus, which makes it harder for sperm to enter the uterus and fertilize the egg, and keeps the lining of the uterus thin, which makes it less likely that a fertilized egg will attach to it.
The IUD has the following benefits:
A health care provider must insert and remove the IUD. He or she will review your medical history and will perform a pelvic exam. To insert the IUD, the health care provider puts the IUD in a slender plastic tube. He or she places the tube into the vagina and guides it through the cervix into the uterus. The tube is withdrawn, leaving the IUD in place.
Insertion of the IUD may cause some discomfort. Taking over-the-counter pain relief medication before the procedure may help. The IUD has a string made of thin plastic threads. After insertion, the strings are trimmed so that 1–2 inches extend past the cervix into your vagina. The strings should not bother you.
With the copper IUD, menstrual pain and bleeding may increase. Bleeding between periods may occur. Both effects are common in the first few months of use. Pain and heavy bleeding usually decrease within 1 year of use.
Both hormonal IUDs may cause spotting and irregular bleeding in the first 3–6 months of use. The amount of menstrual bleeding and the length of the menstrual period usually decrease over time. Menstrual pain also usually decreases.
A few women also may have side effects related to the hormones in these IUDs. These side effects may include headaches, nausea, depression, and breast tenderness.
Serious complications from use of an IUD are rare. However, some women do have problems. These problems usually happen during or soon after insertion:
The birth control implant is a single flexible rod about the size of a matchstick that is inserted under the skin in the upper arm. It releases progestin into the body. It protects against pregnancy for up to 3 years.
The progestin in the implant prevents pregnancy mainly by stopping ovulation. In addition, the progestin in the implant thickens cervical mucus, which makes it harder for sperm to enter the uterus and fertilize the egg. Progestin also keeps the lining of the uterus thin, making it less likely that a fertilized egg will attach to it.
The implant has the following benefits:
The implant is inserted into your arm by a health care provider. A small area on your upper arm is numbed with a local anesthetic. No incision is made. Your health care provider places the implant under the skin with a special inserter. The procedure takes only a few minutes.
To remove the implant, your health care provider again numbs the area. One small incision is made. The implant then is removed.
The most common side effect of the implant is unpredictable bleeding. For some women, these bleeding patterns improve over time. Some women have less menstrual pain while using the implant. In some women, bleeding stops completely. Other common side effects include mood changes, headaches, acne, and depression. Some women have reported weight gain while using the implant, but it is not clear whether it is related to the implant.
Possible risks include problems with insertion or removal of the implant. These problems occur in less than 2% of women. Although rare, if a woman becomes pregnant while the implant is inserted, there is a slightly increased risk that it will be an ectopic pregnancy.
Birth control pills, the birth control patch, and the vaginal birth control ring are combined hormonal birth control methods. They contain two hormones: estrogen and progestin.
Combined hormonal birth control methods release estrogen and progestin into the whole body. These hormones prevent pregnancy mainly by stopping ovulation (the release of an egg from one of the ovaries). They also cause other changes in the body that help prevent pregnancy. The mucus in the cervix thickens, making it hard for sperm to enter the uterus. The lining of the uterus thins, making it less likely that a fertilized egg can attach to it.
With typical use—meaning that the method may not always be used consistently or correctly—9 women out of 100 (9%) will become pregnant during the first year of using these methods. With perfect use—meaning that the method is used consistently and correctly each time—fewer than 1 woman out of 100 will become pregnant during the first year.
Combined hormonal methods have several benefits in addition to protecting against pregnancy:
Combined hormonal methods are safe for most women, but they are associated with a small increased risk of deep vein thrombosis (DVT),heart attack, and stroke. The risk is higher in some women, including women older than 35 years who smoke more than 15 cigarettes a day or women who have multiple risk factors for cardiovascular disease, such as high cholesterol, high blood pressure, and diabetes; a history of stroke, heart attack, or DVT; or a history of migraine headaches with aura.
You should not use combined hormonal methods during the first 3 weeks after delivery because the risk of DVT is higher in the weeks after childbirth. If you have additional risk factors for DVT, you should wait to use combined hormonal methods until after the first 4–6 weeks following delivery.
The risk of DVT also may be slightly higher in women taking pills containing a progestin called drospirenone and in women using the patch. However, the risk of DVT is higher during pregnancy and in the weeks after childbirth than when taking drospirenone-containing pills or using the patch.
If you are breastfeeding, estrogen may affect your milk supply. It is recommended that you wait until the fifth week after delivery to start using these methods, when breastfeeding has been well established.
In the United States, birth control pills are available by prescription only.
Possible side effects include the following:
Breakthrough bleeding usually is a temporary side effect as the body adjusts to a change in hormone levels. It may last longer than a few months with continuous-dose pills.
The vaginal ring is a flexible, plastic ring that is placed in the upper vagina. It releases estrogen and progestin that are absorbed through the vaginal tissues into the body.
A health care provider must prescribe the vaginal ring, but you insert it yourself.
You fold the ring and insert it into the vagina. It stays there for 21 days. You then remove it and wait 7 days before inserting a new ring. During the week the ring is not used, you will have your period. To use the ring as a continuous-dose form of birth control, insert a new ring every 21 days with no ring-free week in between.
Possible side effects include the following:
The contraceptive skin patch is a small (1.75 square inch) adhesive patch that is worn on the skin to prevent pregnancy. The patch releases estrogen and progestin, which are absorbed through the skin into the body.
A health care provider must prescribe the patch, but you do not need to visit a health care provider to apply or remove the patch. The patch is less effective in women who weigh more than 198 pounds.
The patch can be worn on the buttocks, chest (except the breasts),upper back or arm, or abdomen. You wear a patch for a week at a time for a total of 3 weeks in a row. During the fourth week, a patch is not worn, and you will have your period. After week 4, a new patch is applied and the cycle is repeated. You apply the patch on the same day of the week even if you still are bleeding. To use the patch as a continuous-dose form of birth control, apply a new patch every week on the same day without skipping a week.
Most side effects are minor and often go away after a few months of use. Possible side effects include the following:
Progestin is a form of progesterone, a hormone that plays a role in the menstrual cycle and pregnancy. Progestin is used in combination with another hormone called estrogen in combined hormonal birth control pills, the vaginal ring, and the skin patch. It also can be used by itself in progestin-only pills and the birth control injection. The birth control implant and the hormonal intrauterine device also are progestin-only forms of birth control and are discussed
Progestin-only pills and the injection have about the same effectiveness as combination estrogen and progestin pills, rings, and patches.
Progestin-only pills contain progestin. They are available by prescription only.
Progestin-only birth control pills, sometimes called “mini-pills,” have several effects in the body that help prevent pregnancy:
Progestin-only pills may not be a good choice for women who have certain medical conditions, such as some forms of lupus. Women who have breast cancer or who have a history of breast cancer should not take progestin-only pills.
The progestin-only pill comes in packs of 28 pills. All the pills in the pack contain progestin. Take one pill at the same time each day for 28 days. It is important to take the progestin-only pill at the exact same time each day for maximum effectiveness. Do not skip pills for any reason—even if you bleed between periods or feel sick.
If a pill is missed by more than 3 hours, you should take a pill as soon as possible and use a backup method of contraception (such as condoms) for the next 2 days. If vomiting or severe diarrhea occurs within 3 hours after taking a pill, the progestin may not be absorbed completely by your body. Keep taking your pills, but use a backup method until 2 days after your vomiting or diarrhea stops.
Bleeding may be unpredictable. You may have short cycles of bleeding, spotting, or heavy bleeding or no bleeding at all. Other side effects include headaches, nausea, and breast tenderness.
The birth control injection is an injection of the hormone depot medroxyprogesterone acetate. It provides protection against pregnancy for 3 months.
The injection has several effects that work together to prevent pregnancy:
A health care provider must give the injection. The first shot can be given at any time during your menstrual cycle as long as you and your health care provider are reasonably sure you are not pregnant.
You must return to your health care provider every 13 weeks for repeated injections. The repeat injection can be given up to 2 weeks late (15 weeks from the last injection). If it is given more than 2 weeks late, you will need to avoid sexual intercourse or use a backup method of birth control, such as condoms, for the next 7 days.
It has several health benefits not related to birth control:
Bone loss may occur while using the birth control injection. When the injections are stopped, at least some and sometimes all of the bone that is lost is gained back. Women who have multiple risk factors for cardiovascular disease may be at increased risk of cardiovascular disease while using the injection. This increased risk may last for some time after the method is stopped. Women with a history of stroke, vascular disease, or poorly controlled high blood pressure also may be at increased risk of cardiovascular disease while using this method.
The injection may cause irregular bleeding. Some women report weight gain while using progestin-only birth control methods. Among women who gained weight, the average amount of weight gained was less than 5 pounds. It takes an average of 10 months for pregnancy to occur after stopping the injection.
Emergency contraception is the use of certain methods to prevent pregnancy after a woman has had sex without birth control, if her current method fails, or if she is raped.
There are two forms of emergency contraception available in the United States: 1) emergency contraceptive pills and 2) the copper intrauterine device (IUD).
There are three types of emergency contraceptive pills: 1) progestin-only pills, 2) combination pills, and 3) ulipristal.
Progestin-only emergency contraception pills are available as a single pill or two pills that are taken 12–24 hours apart. The pills should be started as soon as possible after having unprotected sex. Progestin-only pills can be used more than once, even within the same menstrual cycle.
Progestin-only pills are thought to prevent pregnancy mainly by preventing ovulation. They will not work if you are already pregnant and will not affect a pregnancy that has started. They are about 75% effective in preventing pregnancy. Their effectiveness decreases with time.
They are most effective when taken within 72 hours (3 days) of unprotected sex. They are moderately effective when taken within 120 hours (5 days).
Birth control pills that contain estrogen and progestin are called combination pills.
Taken in higher-than-usual amounts, combination birth control pills can be used for emergency contraception. They are taken in two doses. The number of pills needed for emergency contraception is different for each brand of pill. Combination emergency contraceptive pills need to be taken as soon as possible up to 120 hours, or 5 days, after unprotected intercourse. They are thought to work by preventing ovulation.
Combination emergency contraceptive pills are not as effective in preventing pregnancy as progestin-only pills. For this reason and because of the higher risk of nausea and vomiting, progestin-only methods are preferred over combination emergency contraceptive pills.
Ulipristal can be taken up to 120 hours (5 days) after unprotected intercourse with no decrease in effectiveness. Ulipristal is available by prescription only. Research suggests that it may prevent more pregnancies than progestin-only pills when taken as directed.
Because the effects of repeated use of ulipristal are not yet known, it should be taken only once during a menstrual cycle. It also may decrease the effectiveness of hormonal birth control methods. For this reason, a nonhormonal method, such as a condom, should be used after taking ulipristal until your next menstrual period starts.
Ulipristal and combination birth control pills are available only by prescription. Plan B One-Step is a progestin-only pill that can be bought at a pharmacy without a prescription. Next Choice One Dose is a progestin-only pill that can be bought at a pharmacy without a prescription if you are 17 years or older and show proof of age and by prescription only if you are younger than 17 years.
You can go to http://eclocator.not-2-late.com or call the Emergency Contraception Hotline (888-NOT- 2-LATE) to find a health care provider who can provide a prescription. Also, many health care providers will give an advance prescription for emergency contraception.
Nausea and vomiting may occur after taking the progestin-only and combination pills. Your next menstrual period may not occur at the expected time. You may have bleeding or spotting in the week or month after the treatment.
Other possible side effects include the following:
These side effects usually go away within a few days. Possible ulipristal side effects include headache, nausea, and abdominal pain. Your menstrual period may occur earlier or later than expected. Spotting may occur.
The progestin-only pills and the combination birth control pills are safe even for women who normally are cautioned against using hormonal birth control methods.
Emergency contraception is used for a much shorter period of time than regular use of a hormonal birth control method. However, these pills should not be used as long-term birth control because frequent use of emergency contraception results in more side effects.
No other tests or procedures are needed after taking emergency contraception. However, you should see your health care provider for a pregnancy test if you have not had a period within a week of when you expect it.
Progestin-only pills and combination pills do not harm a pregnancy or the health of the baby if you are already pregnant. Currently, there is little information about whether ulipristal can harm a pregnancy if you are already pregnant.
It is possible to become pregnant later in the same menstrual cycle if you have used emergency contraception pills. To prevent pregnancy, you should use a barrier contraception method, such as a condom, until your next menstrual period occurs.
You also can start birth control pills, the patch or the vaginal ring immediately after taking emergency contraception, but you also need to use a barrier method until your next menstrual period starts.
The copper IUD must be inserted within 5 days of having unprotected sex. It is about 99% effective in preventing pregnancy. A benefit is that the IUD then can be used for long-term birth control. A drawback is that it does not protect against STDs. If you are at risk of STDs, a male or female condom should be used in addition to the IUD for STD protection. Also, some women with certain medical conditions cannot use an IUD.
Sterilization is a permanent method of birth control. Sterilization procedures for women are called tubal occlusion. The procedure for men is called vasectomy.
Tubal occlusion closes off the fallopian tubes. This prevents the egg from moving down the fallopian tube to the uterus and keeps the sperm from reaching the egg.
Sterilization is a highly effective way to prevent pregnancy. Fewer than 1 out of 100 women will become pregnant within 1 year of having the procedure. After 10 years, pregnancy rates range from fewer than 1 to fewer than 4 out of 100 women, depending on the type of sterilization method used.
Female sterilization does not protect against sexually transmitted infections (STIs),including human immunodeficiency virus (HIV). A male or female condom should be used to protect against these infections if you are at risk of getting an STI
A risk common to all female sterilization methods is that if pregnancy does occur, there is an increased chance that it will be an ectopic pregnancy. However, the risk of ectopic pregnancy occurring in women after tubal sterilization is lower than in women who do not use any birth control. Other risks are specific to the type of procedure.
There are three ways that sterilization for women can be performed:
Minilaparotomy: A small incision is made in the abdomen. The fallopian tubes are brought up through the incision. A small section of each tube is removed, or both tubes can be removed completely. Less often, clips are used to close off the tubes. This approach frequently is used for postpartum sterilization.
Laparoscopy: This is a type of surgical procedure that uses a device called a laparoscope to view the pelvic organs). The fallopian tubes are closed off using instruments passed through the laparoscope or with another instrument inserted through a second small incision.
Hysteroscopy: Hysteroscopic sterilization does not require incisions in the skin. It can be done with local anesthesia in a health care professional’s office (see Small devices are placed into the openings of the fallopian tubes. The devices cause scar tissue to form that blocks the fallopian tubes.
After having the procedure, it takes 3 months for the scar tissue to form. During this time, you must use another form of birth control to prevent pregnancy. A test called hysterosalpingography must be done to ensure that the tubes are blocked before you can use it as your only method of birth control.
The vas deferens is one of two tubes that carry sperm from the testes. In a vasectomy, these tubes are tied, cut, clipped, or sealed to prevent the release of sperm. This prevents a woman’s egg from being fertilized with the man’s sperm.
The effectiveness of vasectomy in preventing pregnancy after 1 year is slightly higher than that of female sterilization. As with female sterilization, vasectomy does not protect against STIs.
One or two small openings are made in the skin of the scrotum. Each vas deferens is pulled through the opening until it forms a loop. A small section is cut out of the loop and removed. The two ends are tied and may be sealed with heat.
This causes scar tissue to grow and block the tubes. Each vas deferens then is placed back into the scrotum. There also is a “no-scalpel” technique that does not require incisions in the skin. It can be done with local anesthesia in a health care provider’s office.
It takes about 2–4 months for the semen to become totally free of sperm. A couple must use another method of birth control or avoid sexual intercourse until a sperm count confirms that no sperm are present. In this test, the number of sperm in a semen sample is counted.
Vasectomy generally is considered to be safer than female sterilization and requires only local anesthesia. Also, there is no increased risk of ectopic pregnancy if the vasectomy fails. Risks of vasectomy include minor bleeding and infection. Major complications are rare.
Sterilization is permanent birth control and is not meant to be reversible. Before having the procedure, you (and your partner, if appropriate) must be certain that you do not want children in the future.
If you have a sterilization procedure and you change your mind after the operation, you can have surgery to try to reverse it, or assisted reproductive technology can be used to attempt pregnancy. These procedures are expensive and may not be covered by insurance. There also is no guarantee that you will be able to become pregnant afterward.